Navigating The Path Home: A Comprehensive Examination Of Discharge Criteria In Healthcare
Navigating the Path Home: A Comprehensive Examination of Discharge Criteria in Healthcare
Related Articles: Navigating the Path Home: A Comprehensive Examination of Discharge Criteria in Healthcare
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Navigating the Path Home: A Comprehensive Examination of Discharge Criteria in Healthcare. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating the Path Home: A Comprehensive Examination of Discharge Criteria in Healthcare

The journey of a patient through the healthcare system is often a complex and multifaceted one, marked by periods of intense treatment and careful monitoring. As a patient’s condition improves, the ultimate goal becomes a safe and successful transition back to their home environment. This transition, known as discharge, is not simply a matter of leaving the hospital or clinic; it is a carefully orchestrated process guided by established criteria designed to ensure the patient’s continued well-being and minimize the risk of readmission. These criteria, collectively referred to as "discharge criteria," represent a vital component of patient care, playing a crucial role in the successful conclusion of the healthcare journey.
Defining the Discharge Criteria:
Discharge criteria encompass a range of factors that healthcare professionals consider to determine when a patient is ready to leave the hospital or other healthcare setting. These criteria are not static but evolve based on the patient’s individual needs, the nature of their illness or injury, and the complexities of their treatment. The primary aim of discharge criteria is to ensure that the patient possesses the necessary level of stability, functional capacity, and support network to thrive in their home environment.
Key Components of Discharge Criteria:
Discharge criteria are typically structured around several key components, each of which contributes to the overall assessment of a patient’s readiness for discharge. These components include:
-
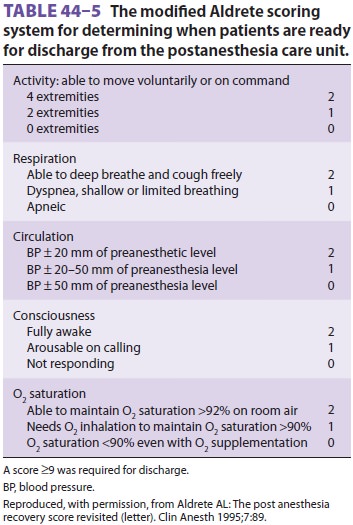
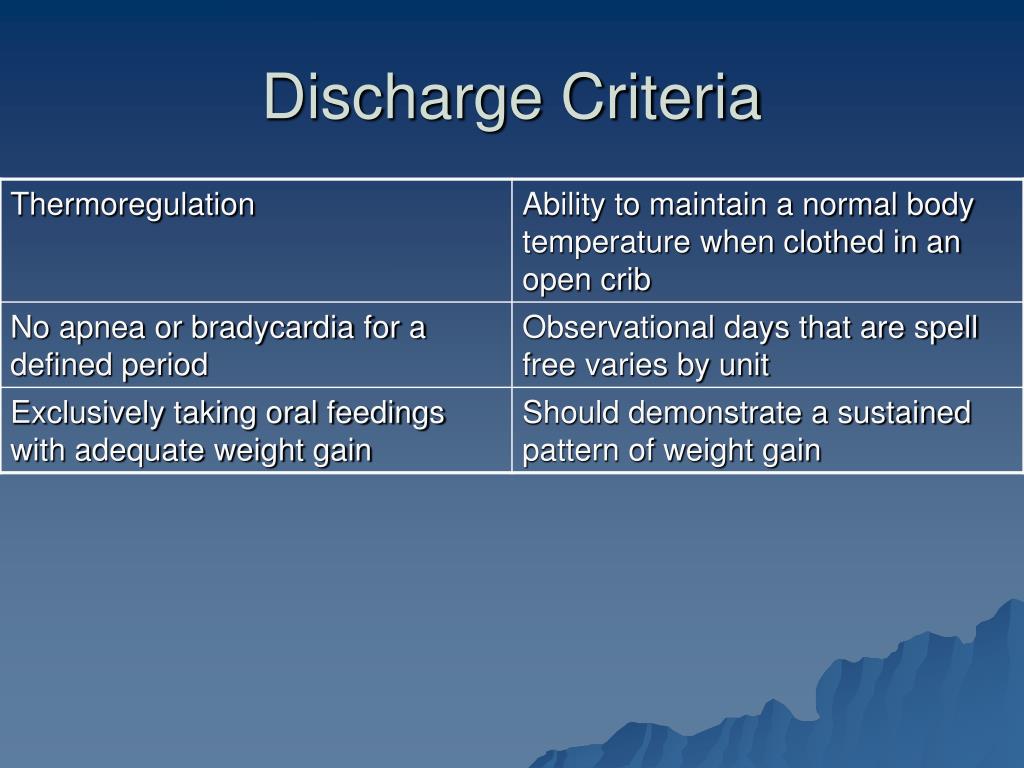
Clinical Stability: This refers to the patient’s physiological condition and the extent to which their illness or injury has been addressed. Indicators of clinical stability may include:
- Stable vital signs: Blood pressure, heart rate, temperature, and respiration within acceptable ranges.
- Controlled symptoms: Pain, nausea, fever, or other symptoms managed effectively.
- Resolved infection: If present, the infection has been eradicated or effectively treated.
- Improved mobility: The patient can move safely and independently, or with appropriate assistance.
-
Functional Capacity: This component assesses the patient’s ability to perform essential activities of daily living (ADLs) such as bathing, dressing, eating, and toileting. Discharge criteria may require the patient to demonstrate:
- Independent ADL performance: The patient can perform ADLs without significant assistance.
- Safe ambulation: The patient can walk safely and independently, or with appropriate assistive devices.
- Cognitive function: The patient possesses adequate cognitive abilities to make informed decisions about their care and manage their medications.
-
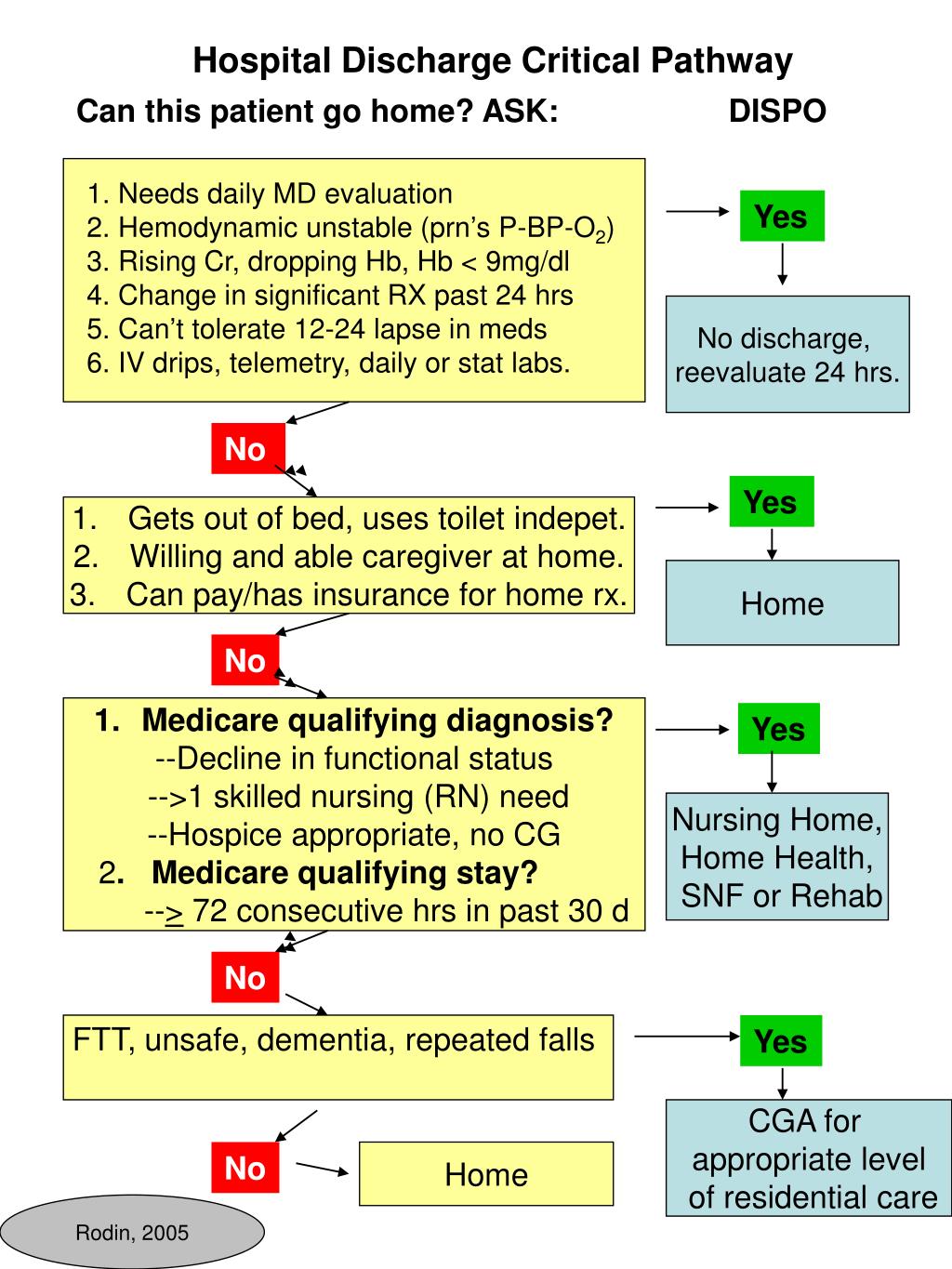
Social Support: This element considers the patient’s support system, encompassing the individuals who will assist them in their recovery and daily life after discharge. Discharge criteria may include:
- Adequate housing: The patient has a safe and suitable home environment.
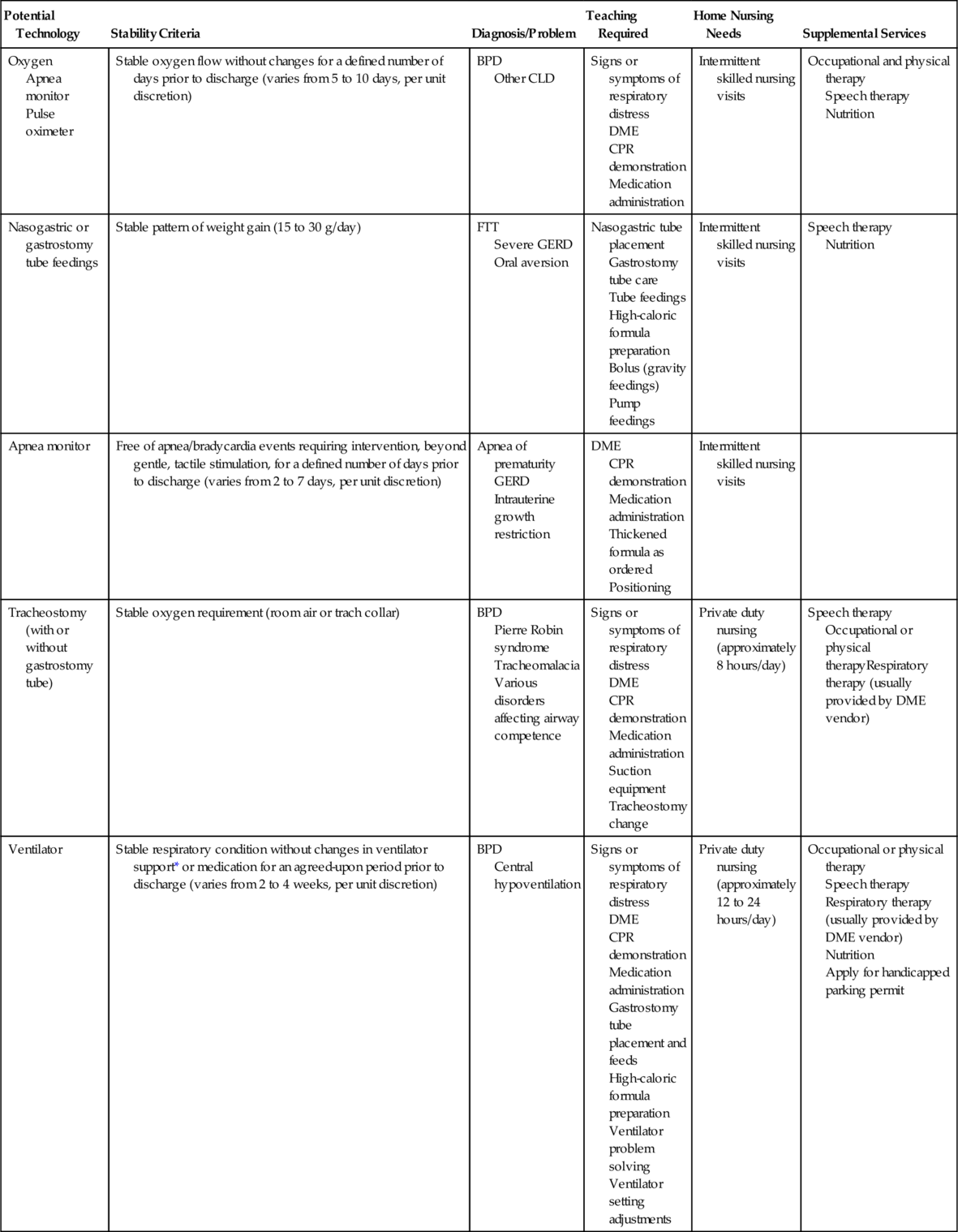
- Reliable caregiver: A family member, friend, or professional caregiver is available to provide necessary support.
- Access to resources: The patient has access to essential resources such as transportation, medication, and medical supplies.
-
Follow-up Care: Discharge criteria often include provisions for ongoing medical care and monitoring to ensure a smooth transition and prevent complications. This may involve:
- Scheduled appointments: Follow-up appointments with physicians, therapists, or other healthcare professionals.
- Medication management: Clear instructions on medication dosages, administration, and potential side effects.
- Rehabilitation services: Access to physical therapy, occupational therapy, or other rehabilitation services as needed.
The Importance of Discharge Criteria:
The significance of discharge criteria extends beyond simply ensuring a patient’s safe return home. They play a crucial role in:
- Improving patient outcomes: By ensuring a patient’s readiness for discharge, these criteria help to prevent complications, reduce the risk of readmission, and promote optimal recovery.
- Optimizing resource utilization: Discharge criteria contribute to efficient use of healthcare resources by minimizing unnecessary hospital stays and facilitating a timely transition to appropriate post-discharge care.
- Enhancing patient satisfaction: A well-defined and effective discharge process can enhance patient satisfaction by ensuring a smooth and coordinated transition to home, minimizing anxieties and fostering a sense of confidence in their recovery.
- Promoting continuity of care: Discharge criteria facilitate a seamless transition between hospital and community care settings, ensuring that patients receive the necessary support and follow-up care they require.
Discharge Planning: A Collaborative Process:
The discharge planning process is a collaborative effort involving the patient, their family, and a multidisciplinary team of healthcare professionals. This team may include physicians, nurses, social workers, pharmacists, therapists, and other specialists.
Key Steps in Discharge Planning:
- Assessment: The healthcare team conducts a comprehensive assessment of the patient’s clinical status, functional capacity, social support network, and need for post-discharge care.
- Goal Setting: The team works with the patient and their family to establish realistic goals for their recovery and post-discharge care.
- Education: The patient and their family receive education about their condition, medications, follow-up care, and any necessary precautions.
- Coordination of Services: The team coordinates with community-based resources to ensure the patient’s access to essential services such as home healthcare, transportation, and medication assistance.
- Discharge Instructions: The patient receives clear and concise discharge instructions outlining their medications, follow-up appointments, and any necessary precautions.
Navigating the Discharge Process:
For patients and their families, the discharge process can be a complex and often overwhelming experience. To navigate this process effectively, it is essential to:
- Communicate openly: Discuss any concerns or questions with the healthcare team.
- Actively participate: Engage in the discharge planning process and advocate for your needs.
- Ask for clarification: Seek clarification on any aspect of your discharge plan that is unclear.
- Utilize available resources: Reach out to social workers, case managers, or other support services for assistance.
Challenges and Considerations:
While discharge criteria serve as a valuable framework for guiding the transition to home, certain challenges and considerations may arise:
- Individualized needs: Discharge criteria must be adapted to the unique needs of each patient, taking into account their medical history, functional limitations, and support system.
- Social determinants of health: Factors such as socioeconomic status, access to transportation, and availability of affordable housing can influence a patient’s ability to meet discharge criteria.
- Readmission rates: Despite efforts to optimize discharge criteria, readmission rates remain a concern, highlighting the need for ongoing research and innovation in discharge planning.
FAQs Regarding Discharge Criteria:
1. What happens if a patient does not meet the discharge criteria?
If a patient does not meet the discharge criteria, they may require additional medical care, rehabilitation services, or support to achieve the necessary level of stability and function before they can be safely discharged.
2. Can discharge criteria be modified for specific patients?
Yes, discharge criteria can be modified based on a patient’s individual needs and circumstances. The healthcare team will work with the patient and their family to determine the most appropriate discharge plan.
3. What are the consequences of premature discharge?
Premature discharge can lead to complications, increased healthcare costs, and a higher risk of readmission.
4. Who is responsible for developing and implementing discharge criteria?
Discharge criteria are typically developed by a multidisciplinary team of healthcare professionals, including physicians, nurses, social workers, and case managers.
5. How can I learn more about discharge criteria for my specific condition?
You can discuss your discharge plan with your healthcare team, including your physician, nurse, and case manager. They can provide you with specific information about the discharge criteria relevant to your situation.
Tips for Successful Discharge Planning:
- Ask questions: Do not hesitate to ask your healthcare team questions about your discharge plan and any concerns you may have.
- Be an active participant: Engage in the discharge planning process and advocate for your needs.
- Communicate with your family: Keep your family informed about your discharge plan and involve them in the process.
- Utilize available resources: Reach out to social workers, case managers, or other support services for assistance.
- Follow discharge instructions carefully: Adhere to your medication schedule, follow-up appointments, and any other instructions provided by your healthcare team.
Conclusion:
Discharge criteria represent a cornerstone of patient care, ensuring a safe and successful transition from the hospital or clinic to the home environment. By carefully considering a patient’s clinical status, functional capacity, social support network, and need for ongoing care, these criteria contribute to improved patient outcomes, optimized resource utilization, and enhanced patient satisfaction. As the healthcare landscape continues to evolve, a focus on personalized discharge planning and the development of innovative strategies to address the challenges associated with discharge will remain essential to ensure the well-being of patients as they navigate the path back home.



Closure
Thus, we hope this article has provided valuable insights into Navigating the Path Home: A Comprehensive Examination of Discharge Criteria in Healthcare. We appreciate your attention to our article. See you in our next article!